By Bel Heaton
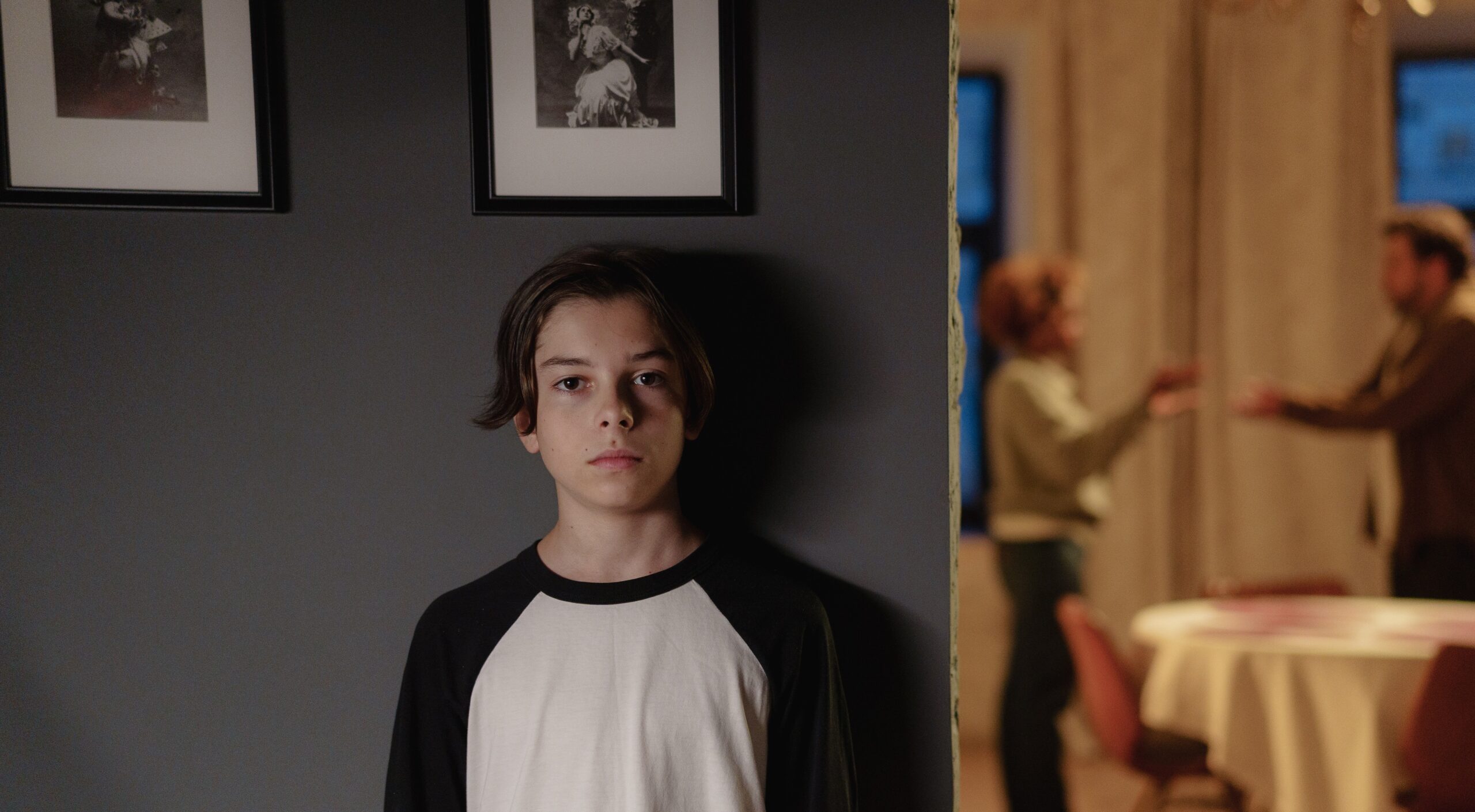
“…looking back, I think if someone at that time would’ve just said, No, just told me no… Maybe I wouldn’t be where I am today”
Luka Hein
These are the words of Luka Hein, a young woman who had both breasts removed at age 16.
Luka is one of a growing number of detransitioners who are living proof that every child who walks into a gender clinic requires careful evaluation before receiving treatment.
Despite the pain and loss that results from the premature affirmation of child gender patients, NSW’s proposed Conversion Practices Prohibition Bill contains restrictions that will make it nearly impossible for parents or clinicians to say ‘no’ or even, ‘wait a little longer’, to young patients.
These laws, introduced by Independent MP Alex Greenwich, may be well-intentioned but in practice, are pathologically altruistic.
In order to understand how ‘anti-gender-conversion’ laws do more harm than good, we should look at how similar laws in other states are interacting with Gender Theory and Australia’s Standards of Care to create a closed loop of affirmation that defies common sense, sound medical judgement and violates patient and parental rights.
The subjectivity of gender Identity
Australia’s Standards of Care define gender identity as, “A person’s innermost concept of self as male, female.” Other definitions are equally theoretical. Materials from Australian school curricula instruct children that that gender identity is simply, “how you feel”.
But the subjectivity of gender-identity, which lies at the core of gender theory, presents parents, clinicians and child gender patients with a problem ; there is no test, comparative standard or empirical proof of a person’s ‘gender-identity’.
This is a problem in need of a considered solution. Around Australia, clinics that once saw children in the single digits now have waiting lists of hundreds. Last year 1,095 children sought help at the Royal Melbourne Children’s Hospital alone (that number represents a 4000% rise in referrals to the hospital over the last 10 years).
Australia’s clinical standards
Australia’s gender clinics rely heavily on two main standards of care; The Australian Standards of Care and Treatment Guidelines (ASOCTG) and the Australian Informed Consent Standards for gender affirming hormone therapy.
Both standards:
- prescribe a Gender Affirming approach, meaning that clinicians should always support a patient’s belief that they may be the opposite sex
- caution clinicians that not affirming patients causes harm
- refer to patients as ‘trans or gender diverse’ throughout, arguably presupposing the diagnosis before a diagnosis is made
Both standards also stress that the best authority on a child’s gender care is the child themselves. As the ASOCTG guidelines say,
“…decision making should be driven by the child or adolescent wherever possible”
ASOCTG, p5.
Criticisms of Affirmation Only standards are often reflexively dismissed as anti-trans dog whistling, but the, high rates of trauma, mental health issues, same-sex attraction and neurodivergence observed in gender patients (in addition to the Standard’s own acknowledgement that some treatments can cause sterility) all demand that child patients receive proper, therapeutic evaluation.
Dr Jillian Spencer, a senior Australian child and adolescent psychiatrist has described how Gender Affirming models severely constrain clinicians’ ability to explore other possible causes of a child’s distress,
“We entered our field to try to assist children to thrive, but the gender clinics have been set up, and psychiatrists are being forced to affirm the social transition of all children…”
“I would say that the vast majority of child and adolescent psychiatrists hold very serious concerns about the affirmation model but to speak up in the current climate or even to take a more cautious clinical approach puts their employment at risk, their AHPRA registration is at risk and they fear criminal sanctions under the conversion therapy laws in some states.”
Most transgender interest groups also openly endorse Gender Affirming care. TransHub, for example provides a list of Gender Affirming Doctors alongside a list of questions to help children determine if a practitioner is likely to affirm them. There is also no dearth of social media accounts instructing on how to best access gender affirmation and the treatments it entails.
Like detransitioner Ollie Davies, many children who seek out gender clinics are gay or bisexual kids struggling with their orientation and who are temporarily seduced by the promise that transition offers the same-sex attracted – the chance to be straight. It’s a horrible irony that by mandating Affirmation Only, ‘anti-gender-conversion’ laws will often lead to gay kids being medically converted into straight kids.
What procedures are children eligible for?
If parental consent is given, children can access puberty blockers, cross sex hormones and certain gender-affirming surgeries.
Australian girls as young as 15 have received double mastectomies. Due to the growing popularity of the procedure, surgeons have called for clearer guidelines and the consideration of age-limits.
The Standards don’t identify a minimum age for treatment.
When parent say no
Clinicians or parents who don’t affirm a child’s gender identity or consent to medical treatment can appeal to the Family Court, but may also find themselves in contention with various state laws.
STATE Legislation
So-called gender ‘suppression or conversion practices’ laws are in effect in Victoria, Queensland, the ACT and are now under consideration in NSW.
These laws criminalise practices that ‘seek to change or suppress a person’s sexual orientation or gender identity’. In the context of sexual orientation, these bans make perfect sense, but for clinicians and parents of gender-questioning children, they effectively criminalise therapy that explores alternative causes for gender-distress.
Former professor of psychology at the University of Sydney, Dr Dianna Kenny has said that these laws have had a chilling effect on clinicians,
“Psychologists in Victoria are terrified of practicing non-affirming psychotherapy for children with gender dysphoria,”
Dr Dianna Kenny
NSW’s proposals also take Victoria’s lead in mandating fines and imprisonment, proposing that NSW residents who engage in a ‘suppression practice‘ could face a maximum of 10 years imprisonment or a fine of $6,000.
State child-protection or human rights legislation can also enforce the mandate to affirm.
In 2021, two Western Australian parents had their child removed from their custody after a court deemed that their failure to affirm their child’s gender identity was emotional abuse.
And Human Rights Victoria provides these examples of prohibited practices:
- a parent rejecting the recommendations of qualified health professionals and refusing to support their child’s request for medical treatment that will prevent physical changes from puberty that do not align with the child’s gender identity because the parent believes it is against nature and a boy should be a boy and a girl should be a girl
- waiting until the child is 18 to permit that child access to professional health advice in the hope that the delay will stop the child’s gender identity or sexual orientation
Notice that these examples would require a court to adjudicate on a parent’s intent.
The Family Court
When children, parents or clinicians disagree on a child’s care, an application can be made to the Family Court of Australia. But those who manage to withstand the cost and the emotional strain of litigation may still find that the Court suffers from a lack of neutrality on the matter of child-gender-care.
Judges are not doctors and therefore, are dependent on the testimony of medical experts. Because the Gender Affirmation model is held up as best practice, affirming practitioners are often the only practitioners considered suitably expert to be consulted with. Prominent family law barrister Belle Lane has written that,“In almost all cases coming before the Court, medical affirmation is presented as the only model.” Manhattan Institute fellow Leor Sapir, who has noticed similar patterns playing out in US courts, has described this circular rationale as a ‘no true Scotsman’ fallacy (Audio: 44 minutes).
It’s also rare for judges to go against the advice of medical experts. A review of case law found that during 2004 and 2022 Family Court judges never took a position contrary to the advice of treating medical practitioners.
While a 2020 Court decision appeared to preserve a degree of discretion for families when it found that both parents must consent before any gender-affirming medical treatment occurs, the way that the Family Court interacts with new state and territory laws on gender affirmation has not yet been properly tested.
It’s worth noting that NSW’s new Bill also proposes that that for children under 16, decisions about medical treatment may be made with the consent of one parent – a stipulation at odds with the Family Courts precedent requiring consent from both.
No one-size-fits-all approach
It isn’t transphobic to recognise that for most people, exploring the relationship between our sexualities, identities and the gender-roles that our cultures places upon us, is the work of decades, if not a lifetime.
Some kids do experience persistent and severe gender dysphoria. For others it desists. But all kids – trans kids, gay kids, tom-boys, neurodivergent kids, or just struggling kids – deserve better than a the ‘one-size-fits-all’ approach of Affirmation Only.
While the desire to affirm transgender children comes from a place of compassion, the medical and legal pathways that are being laid down leave little to no room for differential diagnosis, or for providing children and their families with the necessary time to think.